SETTING UP OF A COMMUNITY BASED PALLIATIVE CARE SERVICE
Many chronically ill people spend most of their time at home and are in need of regular care for the rest of their lives. Unlike the patient with acute illness, inpatient and outpatient units alone can not address these needs. Majority of these patients wish to die at home but barely a quarter manage to do so. For example, over 90% of all patients with cancer spend some time in hospital during the last year of life and more than 70% die in hospital or in a hospice. The desired place of death may change with altered circumstances, the most obvious being difficult symptoms and lack of practical help at home. Patients who are frightened, insecure, or lack confidence in their support network are more likely to seek urgent admission to hospital or hospice. Equally, if informal carers are physically or mentally tired they are more likely to seek admission, even when death is imminent. Across the whole range of health services, an increasing amount of care is being provided on an outpatient basis or through the hospitals. Putting the concept of 'total care' with continuous support in physical, psychosocial, and spiritual realms into practice is very difficult through institutionalized care. It offers a patchy service through which the patient and family has access to care for a few hours/ days. The physical complexities of progressive and life threatening disease, coupled with attendant emotional and psychological consequences, demand careful coordination between primary, secondary, and tertiary care. The community approach is the only realistic model for achieving significant coverage and continuity of services for terminally ill. This is a realistic option in most communities where inter personal relationships have not yet fully died out.
Rationale for a Community approach to Palliative Care Service
Patients with advanced diseases require continuous care and attention for the rest of their lives.
- They are also in need of regular social, psychological and spiritual support in addition to the medical and nursing care.
- Care should be readily accessible and available as close to home as possible.
- There is enough social capital available to build a ‘safety net' in the community around these patients.
Community
The word community is derived from the Latin communitas (meaning the same), which is in turn derived from communis, which means "common, public, shared by all or many".Communis comes from a combination of the Latin prefix com- (which means "together") and the word munis (which has to do with the exchange of services), probably originally derived from the Etruscan word munis- (meaning "to endow", or "to have the charge of"). In biological terms, a community is a group of interacting organisms sharing an environment. In human communities,intent, belief, resources, preferences,needs,risks, and a number of other conditions may be present and common, affecting the identity of the participants and their degree of cohesiveness. Traditionally in sociology, a "community" has been defined as a group of interacting people living in a common location. However, the definition has evolved and been enlarged to mean individuals who share characteristics, regardless of their location or type of interaction. In this sense, "community" can mean a community of interest or an ethnic group. What these various meanings have in common is that they refer to the strength of the ties between the members of the group, of whatever nature—cultural, ethnic, or moral—they may be. When we talk about community, it is important to remember that the community is not monolithic. Each community has a dynamic interaction between different interests – supporting each other, competing with each other and sometimes in conflict with each other.
Community Participation
Community participation can be loosely defined as the involvement of people in a community to solve their own problems. It is a very broad concept and in the context of a program, it can mean anything from simple feedback from the community to major involvement in all the phases and areas of the program. Community based palliative care services are those run with community participation. An ownership of the program with participation of the local community in the need assessment, planning, implementation, resource mobilisation, day to day management and evaluation of the program is desirable. It may not be possible for each and every member of the affected population to contribute to a program equally but attempts can be made to actively involve as many key groups and individuals as possible.
Components of Community Based Palliative Care Services
- Community volunteers
- Health care professionals
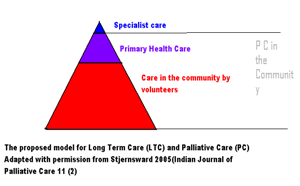
Community volunteers play a major role in the program. Their activities related to the care of the patient and family need to be supported by health care professionals at various levels.
Community Volunteers
A volunteer is someone who works for a community or for the benefit of environment primarily because they choose to do so. Many serve through a non-profit organization – sometimes referred to as formal volunteering, but a significant number also serve less formally, either individually or as part of a group. Volunteering in palliative care may come in many forms: serving food to a starving family, spending time with a lonely patient, mobilizing support for the patient and family from the community, fund raising for the initiative, offering emotional support to the patient and family, providing administrative support to the group etc
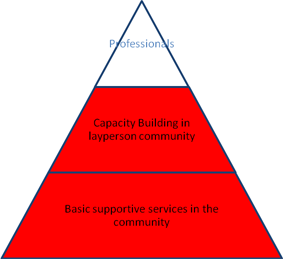
Community volunteer manpower is mainly of two types:
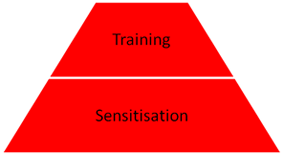
Untrained Sensitized Volunteers
They provide the groundwork for the palliative care service by establishing a social support system eg; food for patients, transport, educational support for children and working with the local government. Such volunteers can be motivated and mobilized by several initial sensitization programs in the community.
Trained Volunteers
Some of the sensitized volunteers undergo a more intensive training program. With proper training, many of them are able to involve in patient care in a bigger way by offering
Health Care Professional Component
The community volunteers need to be supported by health care professionals trained in palliative care. The team should essentially have doctors and nurses, but can also include other health care professionals. Unlike the volunteers from the community, most health care professionals in the team are paid remunerations. This core team can be supplemented with additional voluntary efforts from other health care professionals if available. Nurse led home care should be the key professional service in community palliative care programs. Nurses in the team can be staff nurses with training in palliative care or auxiliary palliative nurses trained for the purpose. Custom made training for local men or women or local health workers is a good option. This service is to be supported by regular medical inputs by doctors and doctors’ led home-based care. This, in addition, can be supplemented by outpatient clinics and inpatient services. A community level care should have a good linking up with a primary, secondary and tertiary health care system for any referral or interdisciplinary support.
Initiation of a Community Based Palliative Care Service
A community based palliative care service is essentially a matrix of four components

The entry point for initiating the service can be any component in the matrix- Starting a community volunteer program, a nurse led home care program or a doctor led outpatient /inpatient / home care unit. Experience has shown that the best option from the point of sustainability is to start with a community volunteer program. Sensitisation of the local community is very often the best possible first step.
Community mobilisation:
Community mobilisation applies to the way in which people can be encouraged and motivated to participate in program activities. In order to mobilise a community successfully it is important to identify Where people’s priority lie and what it is that motivates them.
To raise levels of awareness and sensitisation can be a key aspect of engaging and mobilising a community.
The development of a service in the community can be facilitated by anyone interested in palliative care. To raise levels of awareness and sensitisation can be a key aspect of engaging and mobilising a community.
Community owned services are likely to be successful in any community where people have the willingness to help each other. It is important to make sure that minority groups, low status groups and poorer groups in the community are not left out and that women, men and children are specified in consultation processes. The experience in Kerala has been that people belonging to the lower socio economic strata participate in the program in a more active way than those from upper strata of the society.
Defining a clear ‘catchment area’ and target group for patient care is advisable in the initial phase of the project. These can be expanded later as the project develops.
Beneficiaries:
The patients and families benefit directly from the services. The local community also benefits through enhancement of social capital, improving skills and confidence and the process of empowerment. Building awareness and acceptability to palliative care and developing a more positive outlook towards incurable diseases are also the benefits. The major long term advantage of a community owned project in palliative care is that it makes the community more confident and self sufficient.
Services to be Provided:
The range of services that can be provided through a community based palliative care program are very much in line with the concept of total care in palliative care.
Home care is the mainstay of these services. The home care team consisting of health care professionals and community volunteers visit the patient and family at home, discuss the problems and offer appropriate services. Development of the wider network of community volunteers in the neighbourhood helps ensures continuity of services between home visits and also the necessary social support for the patient and family.
Professionals
Health Care professionals with possible role in community based palliative care services include nurses, doctors, physiotherapists and counsellors. Services of nurses and doctors are essential; others if available can play their roles. The nature of problems of patients with advanced diseases makes nurses with good communication skills the lead professional in home care services.
Community Volunteers
• Educational support for children
• Helping with transport to hospital's
• Linking with other support groups
• Helping to make potential benefits from government / NGOs available
• Rehabilitation
Community volunteers can also take up responsibilities related to organisation and administration of services. Examples included
The home care should be equipped with essential medicines and consumables for their job.
Funds
Community ownership of the program usually ensures good financial support from the community. Community participation can include finance generating activities and this may be a key starting point in giving communities greater responsibility, removing dependence on external support and promoting sustainability. It may be in the form of donation boxes at public places, collections from student community, donations of cash and kind during festive occasions etc. Economic activity through trade and service provision like setting up a small groceries or vegetable shop, tailoring, haircutting saloon etc can also be considered depending on existing skills and needs within the communities.
Fund Raising by Community Owned Palliative Care Units in Kerala – The Strength of Micro Funding
More than 100 palliative care units belonging to the Neighbourhood Network in Palliative Care depends on local donations for their activities. For example, the total recurring expenses for the 28 palliative care units in the district of Malappuram in 2007 was more than three crore rupees. 30% of this budget came as support from Local self Government Institutions in the region. The other 70% (about two crore rupees) was raised locally. 75% of this money (150 lakh rupees) came as donations of less than fifty rupees. Ways to generate funds included
Micro funding: Small donations from large number of people in the community are found to be one of the best ways to ensure sustainability and local ownership to community owned programs.
Where programs are externally assisted like by a non-governmental organisations or philanthropic individuals or trusts, generally the implementing agency takes responsibilities for procuring and managing funds and the community is neither expected to contribute nor have any direct involvement in how this money is spent. Such programs owned by external agencies have the major disadvantage of lack of sustainability once the agency / funder leaves / gets disinterested.
Partnership with the Government
If a program is effective and successful, it is easier to convince the government to integrate it into the mainstream health policy and implementation.
Example 1: In the state of Kerala, at present there are around 130 palliative care units. Majority of them are organized and supported by Community Based Organizations (CBO). Most of them are independent units, but some are based in government and private hospitals. The CBOs are mostly supported by local communities, are self-sustainable in terms of manpower, money and other amenities and dependent on trained volunteers for organizing the services and psychosocial support. In many places, the Local Self Governments Institutions (LSGI) have come forward to work with these groups in providing home visits, outpatient service and free drugs for the poor. Recognizing the need of palliative care as a primary health care and the importance of home care services for patients with long term/ incurable diseases, the Government of Kerala recently brought out a Kerala State Policy for Pain and Palliative Care Services.
Example 2: The National Rural Health Mission (Kerala) has initiated a major project in Kerala this year to facilitate the development and expansion of community owned palliative care services in collaboration with Local self Government Institutions in the state
Recognizing the need of palliative care as a primary health care and as a supportive care for disease specific treatment, the government of Kerala has introduced a Kerala State Policy for Pain and Palliative Care Services.
Example 3: The government of Andhra Pradesh has recently started a health insurance system for people with below poverty line. The insurance also includes palliative care for cancer in the scheme (refer Aaryogyashree Health Care Trust, http://aarogyasri.org).
Training:
Capacity building through skill training and confidence building can be a key ingredient in motivating and mobilising different sections of a community like
It is important to make sure that the health care professionals and community volunteers involved in home care activities have the necessary knowledge, skills and attitude. Various training programs are available for doctors, nurses and community volunteers interested in palliative care.
For the details of training programs being offered in different parts of the country refer to the Indian Association of Palliative care website,http://www.palliativecare.in/training.html) http://www.palliativecare.in/training.htm.
Linking up /integration:
Linking up or the integration with different organisation gives a better sustainability, coverage a better multidisciplinary approach to the program. The home care program can be linked up with organisations/ institutions
Arogya Keralam Projects for Community Based Care of the bed ridden, elderly, chronically and incurably ill in Kerala is an example of integration of a community based palliative care with a state- based central government organisation called National Rural Health Mission(NRHM)
Quality assurance:
1. There should be mechanisms in place for a regular monitoring and feed back. The regular appraisal may consist
2. A Continuous Training / updating program for volunteers and health professionals is essential to raise and maintain the standard of palliative care service delivered. Stagnant programs tend to deteriorate.
3. Outcome Measurement
There is no validated ways of measuring the outcome of a delivery of a community based palliative care. There are several indirect ways of measuring the outcome like patient / family satisfaction surveys, number of volunteers enrolled, number of training and sensitisation programs conducted, coverage, patient population, opioid consumtion, number of rehabilitation programs being implemented, expansion of services, fund generated, governmental involvement etc.
An Action Plan for Initiation of A Palliative Care Service In The Community:
Step I: Sensitisation: In any region, there will be people interested in helping others. Many of them might already have been helping others in their individual capacities. The idea is to sensitise them to the problems of patients with incurable diseases and also to get as many of them together as possible. The first step is to get those who are likely to be interested to an awareness meeting / discussion. Make sure that all the groups / organisations involved in social / health care activities in the region are invited. This meeting should ideally be convened by a ‘neutral’ local group or institution to ensure participation from the different interest groups/ organizations in the region. Explain the issue of incurably ill / bed ridden patients in the region. Discuss possible way to help them. Register those who are willing to spend a couple of hours every week for such patients as volunteers.
Step II: Train those who are willing to get trained in basic nursing care and communication skills / emotional support. The training should be done locally and also at a time and venue convenient to the majority of the participants. (Topics to be covered suggested earlier in this section). Get the trained volunteers to document the problems of bed ridden / incurably ill patients in their neighbourhood (Use a proper form like the community volunteers patient care protocol). It is important to have weekly review meetings of the new volunteers at this stage. These review meetings can be used to discuss solutions to the problems documented by the volunteers. Initiate a social support program to support food for starving families, educational support to the patients’ children, emotional support to patients and families by trained volunteers etc. Establish a contact point for giving and taking information. A space available with one of the new volunteers or well wishers can be used (for example, a local shop, public library premises etc.) Start collecting money, manpower and other resources. Link with the nearest palliative care unit if one is available.
Step III: Adding a nursing component to the program is the next step. It may take 1-2 months for the local group to establish a stable social support system and to raise money to employ a part time nurse. Getting the services of a nurse in the neighbourhood is the best option from the long term point of view. Encourage the nurse to get trained in palliative care. Initiate nurse led home care programs. In certain situations, help from the nurse from a nearby palliative care unit might be available. Use the nurses’ protocol as guide to nurse led home care. Establishing a culture of meticulous documentation and review is important.
Step IV: Getting the medical component in is very often the most difficult part due to ‘scarcity’ of trained doctors. One possible option is to get help from a local doctor in medical issues. Self study by the doctor can be facilitated by regular supply of reading material. Encourage the doctor to get trained in palliative care.
Step V: Once the home care service starts getting established, there will be a need for a regular outpatient clinic. Availability of trained doctor and nurse is a pre requisite. Remember that starting an institution (Outpatient clinic / Inpatient services) is more expensive than initiating a home care program. The facility can very often be linked to a local hospital.
Step VII: Establish a system of regular review and evaluation. Any palliative care or supportive service usually generates good appreciation from the local people. It is important to not to get carried away by the good words. Active attempts at identifying areas for improvement should always be there.
Step VI: Continue with steps I and II